Overview
HarrisLogic’s StellaCARE solution provides 24/7/365 on-demand behavioral health consultations to emergency departments (ED) through telehealth interactions with their patients, staff, and stakeholders. Utilizing proprietary HarrisLogic documentation and decision-support software, our professional clinical staff operate from our virtual care center to enhance and improve an ED’s abilities in the triage, assessment, care plan creation, and coordination of care for their highly challenging mental health cases. StellaCare is a uniquely effective platform that addresses the clinical, operational, and economic demands on the ED presented by this patient population.
Who We Are
Technology
- StellaLOGIC – Novel Behavioral Health Technology
- 24/7 Virtual Care Center
- State of the Art Telepresence
Experience
- 7,000+ Emergency Department Consults
- 2,000,000+ Crisis Encounters
- American Association of Suicidology Accredited
- 12 years providing tele-mental health services
People
- Accredited and Licensed Mental Health Clinicians
- Bachelors, Masters, and PHD’s
- Industry leading training program
StellaCARE empowers emergency departments to manage their behavioral health population more effectively and efficiently; creates capacity to improve throughput and operations; introduces new revenue opportunities; reduces avoidable costs; and minimizes unnecessary inpatient admissions. For patients, we drive better outcomes and experience through timely treatment, more accurate diagnosis and level-of-care determination, and a pathway to achieve success in less restrictive community-based services.
Mental Health Crisis Cycle
The mental health crisis cycle is a vicious loop where individuals perpetually move between the community, emergency departments, hospitals and jails, yet rarely see any health improvements. Ultimately, the mental health crisis cycle creates a wide array of complex and challenging issues:
- High costs associated with unnecessary higher levels of care and ED re-admissions
- Long wait and boarding times for behavioral health patients
- Scarcity of system-wide psychiatric beds
Case Study: Dallas Metro
Across the country, many communities are suffering from dramatic overuse of emergency departments and excessive inpatient psychiatric admissions. In 2011, North Texas began to experience a significant increase in emergency department visits by consumers presenting with co-occurring behavioral health and substance-use related disorders. Like many health systems, the region was beset by a crisis cycle that was driving increased costs and poor clinical results.
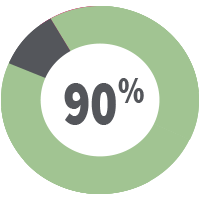
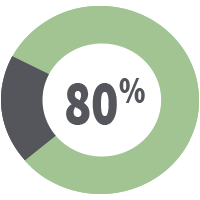
To meet the needs of the Dallas region, the local behavioral health authority tasked HarrisLogic with developing a solution to improve level of care determinations to ensure that patients were treated in the least restrictive setting possible. After 13 months, and more than 7,000 evaluations spread across 11 hospital systems and their 29 emergency departments, HarrisLogic has maintained a diversion rate of 80%. This metric represents an estimated 20-30% improvement when compared to prior years. All of this was achieved while simultaneously reducing ED dwell times and improving outpatient connection rates.
Key Features and Benefits
Patients
- Improved access to timely, quality care
- Engagement in community-based care
- Greater likelihood of successful long-term outcomes
Emergency Department
- Operational efficiency
- Focus on cases within core competencies
- Reduced distraction and risk
- Improved metrics/lower readmissions
Health System
- Cost reductions
- New billing opportunities
- Reduced inpatient capacity utilization by BH
- Leveraged 3rd party on demand capabilities


